
Virus Watch preliminary findings on 8th July 2024
You can find our most recent results at findings so far.
Virus Watch is a research study run by University College London and the NHS. The study aims to identify how COVID-19 spreads, and how to stop it. Findings so far presented on this page are early, preliminary results and should be interpreted with caution as they have not all yet been peer-reviewed by scientists external to our research collaborators. We are presenting these early findings for participants, the general public and policy makers. A detailed description of the Virus Watch study and our research questions can be found in our study protocol. Virus Watch began recruiting people in June 2020 and since then, 58,628 people in 28,527 households across England and Wales have joined the study. You can find a detailed description of the cohort in a profile of the study here.
Table of contents
- Summary of findings
- Barriers in accessing healthcare during the COVID-19 pandemic
- Antibody Trajectories in People with Post-Covid Condition (Long Covid) versus Acute-Only Infections
1. Summary of findings:
Barriers in accessing healthcare during the COVID-19 pandemic.
- There is evidence of inequities in accessing healthcare by minoritised groups prior to the pandemic and further evidence indicated that this gap has widened during the pandemic.
- Using data from Virus Watch, we estimated the proportion of participants who reported difficulty accessing healthcare as well as the distribution of reasons given for this.
- Minority ethnic individuals and those living in deprived areas were more likely experience barriers to accessing healthcare during the COVID-19 pandemic compared to White British participants and those living in the least deprived areas in England and Wales. The most frequently reported barriers by these populations were ‘insufficiently flexibility of appointments’ and ‘not enough time to explain complex needs’.
- This study suggests that it is essential these barriers are addressed as services seek to manage backlogs of care and to ensure equitable healthcare access.
Antibody Trajectories in People with Post-Covid Condition (Long Covid) versus Acute-Only Infections.
- The way people’s immune system responds to infection may be different in people who develop Long Covid compared to those who do not
- We looked at whether antibody levels related to SARS-CoV-2 infection and Covid vaccinations were different in people who developed Long Covid compared to people who did not
- People with Long Covid had higher infection-related (anti-nucleocapsid) antibody levels for the year after infection compared to people who recovered fully
- We did not find any differences in antibody responses to vaccination, only to infection
2. Barriers in accessing healthcare during the COVID-19 pandemic
The COVID-19 pandemic highlighted existing inequalities in healthcare access particularly among minoritised groups such as ethnic minorities, migrants and those living in deprived areas. Such differential barriers to accessing healthcare contribute to inequitable health outcomes.
We used data from a Virus Watch survey (January 2022) on healthcare access in the previous year to describe the characteristics of individuals who experienced barriers, and identify what those barriers were. Of the 12,237 participants who reported having tried to access healthcare in 2021, 4,571 (37.4%) reported difficulties accessing healthcare.
We found a higher proportion of participants from minority ethnic backgrounds reported difficulties accessing healthcare than White British participants (41.6% vs. 37.1%). Similarly, participants residing in the most deprived IMD quintile (1st) also reported barriers to accessing healthcare more frequently than those in the least deprived (5th) (45.5% vs. 35.5%). Migrants and non-migrants reported difficulty accessing healthcare at broadly similar levels.
When accounting for age and sex, we found that UK-born participants who were of minority ethnicity were 40% more likely to report barriers accessing healthcare than White British UK-born participants.
Figure 1. Percentage of participants in minority ethnic and white British groups who selected each barrier to healthcare access. Figure purposely excludes the most commonly selected reason, “Services having been disrupted or cancelled due to the COVID-19 pandemic” so as to better illustrate the differences between the remaining top ten selected barriers.
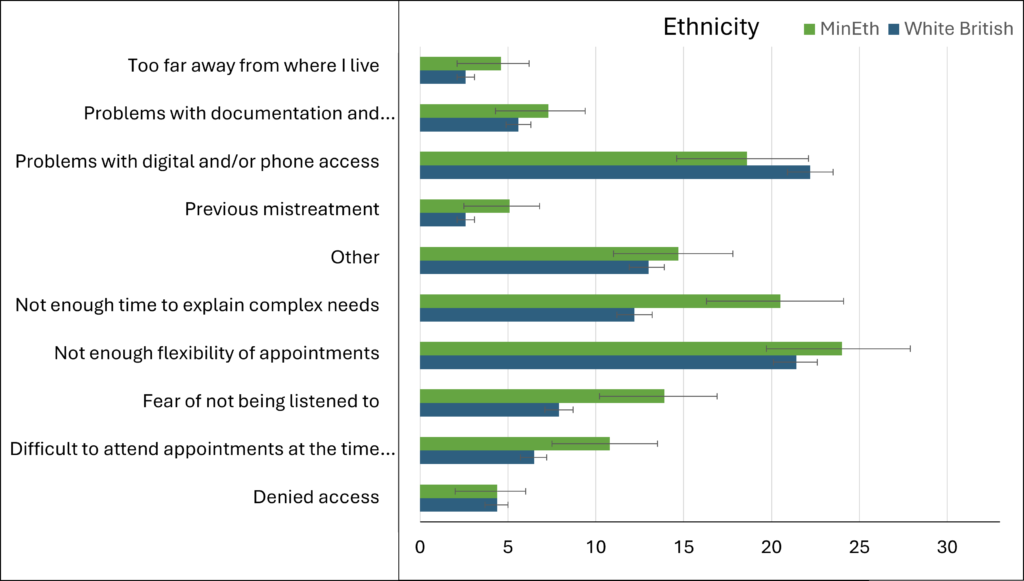
Figure 2. Percentage of UK born and not UK Born groups who selected each barrier to healthcare access. Figure purposely excludes the most commonly selected reason, “Services having been disrupted or cancelled due to the COVID-19 pandemic” so as to better illustrate the differences between the remaining top ten selected barriers.
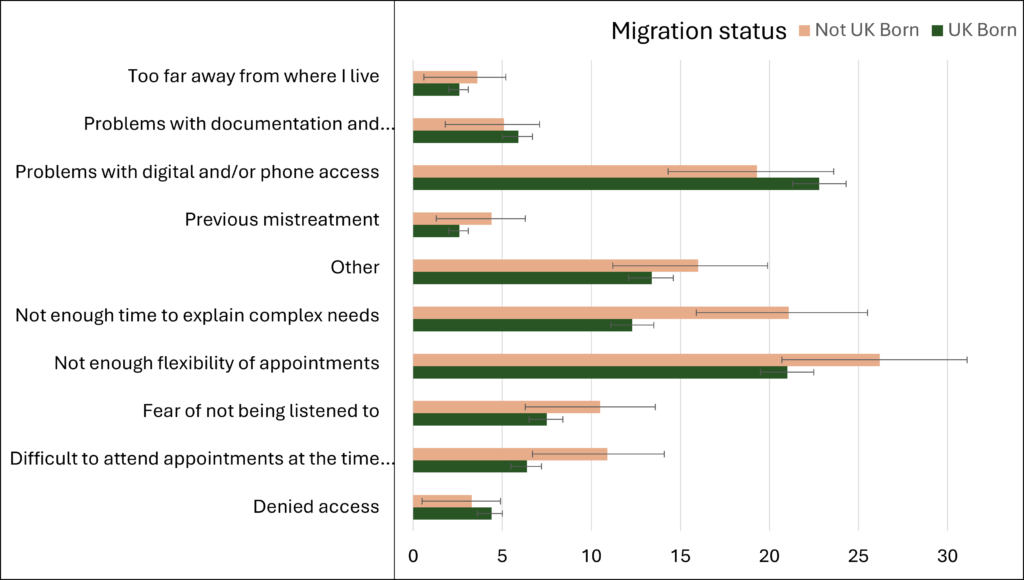
Figure 3. Percentage of participants residing in 1st and 5th IMD quintile who selected each barrier to healthcare access. Figure purposely excludes the most commonly selected reason, “Services having been disrupted or cancelled due to the COVID-19 pandemic” so as to better illustrate the differences between the remaining top ten selected barriers.
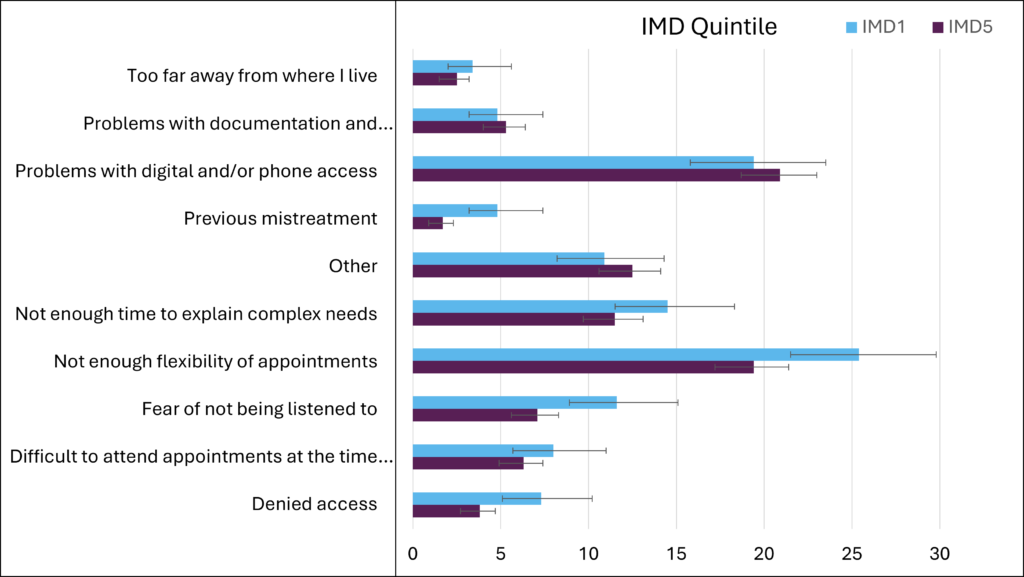
Overall, the most commonly reported barrier was “services disrupted or cancelled due to the COVID-19 pandemic” (72.0%, 3,291/4,571). As seen in figure 1, we also found that participants from minority ethnic backgrounds were more likely than their White British counterparts to report difficulty attending appointments at the times they were offered (10.7% vs. 6.5%) and fear of not being listened to (13.9% vs. 7.9%). Migrants were more likely than non-migrants to cite not having enough time to explain complex needs (21.1% vs. 12.2%) (Figure 2). Participants residing in the most deprived (1st) IMD quintile also had a higher likelihood to cite fear of not being listened to (11.6% in the 1st vs. 7.1% in the 5th) and being denied access (7.3% in the 1st vs. 3.8% in the 5th) than those living in the least deprived (5th) IMD quintile (Figure 3).
This study highlights a need to ensure that people from minoritised populations can present to health services without these fears and concerns. As services continue to manage ever present backlogs of care, it is essential these inequities in access are examined comprehensively together, and that the barriers are addressed.
3. Antibody Trajectories in People with Post-Covid Condition (Long Covid) versus Acute-Only Infections
While most people recover from SARS-CoV-2 infection without any complications, between 10-30% of people develop long-term symptoms even after mild-moderate infections. An important scientific hypothesis or theory is, whether developing long-term symptoms (Long Covid) is associated with how your immune system responds to SARS-CoV-2 infection. Antibodies are proteins that our body makes after infections or vaccinations that help our immune system to protect us. In this study, we aimed to look at whether SARS-CoV-2 antibody levels were different in people with and without Long Covid. We also looked at whether antibody responses to vaccination were different in people with and without Long Covid. This is the largest study of its kind to date.
We used data from a subgroup (n=2010) of people in Virus Watch who completed monthly finger prick antibody tests between February 2021 and March 2022, had a SARS-CoV-2 infection during this time, and completed surveys about long-term symptoms afterwards. We compared antibody levels between people with and without Long Covid over time. People with Long Covid had higher levels of antibodies that respond to infection (anti-nucleocapsid antibodies) for the year after infection compared to people who recovered fully (see Figure 1 below). This shows that people who developed Long Covid in our study had different immune responses to infection compared to people who did not. We found that antibody responses to vaccination (anti-spike antibodies) did not differ between people with and without Long Covid. This was true both before and after infection. We could only follow study participants for one year so we do not know what happened after this period of time.
Figure 1. Infection-Related (Anti-Nucleocapsid) Antibody Levels over Time in People With and Without Long Covid
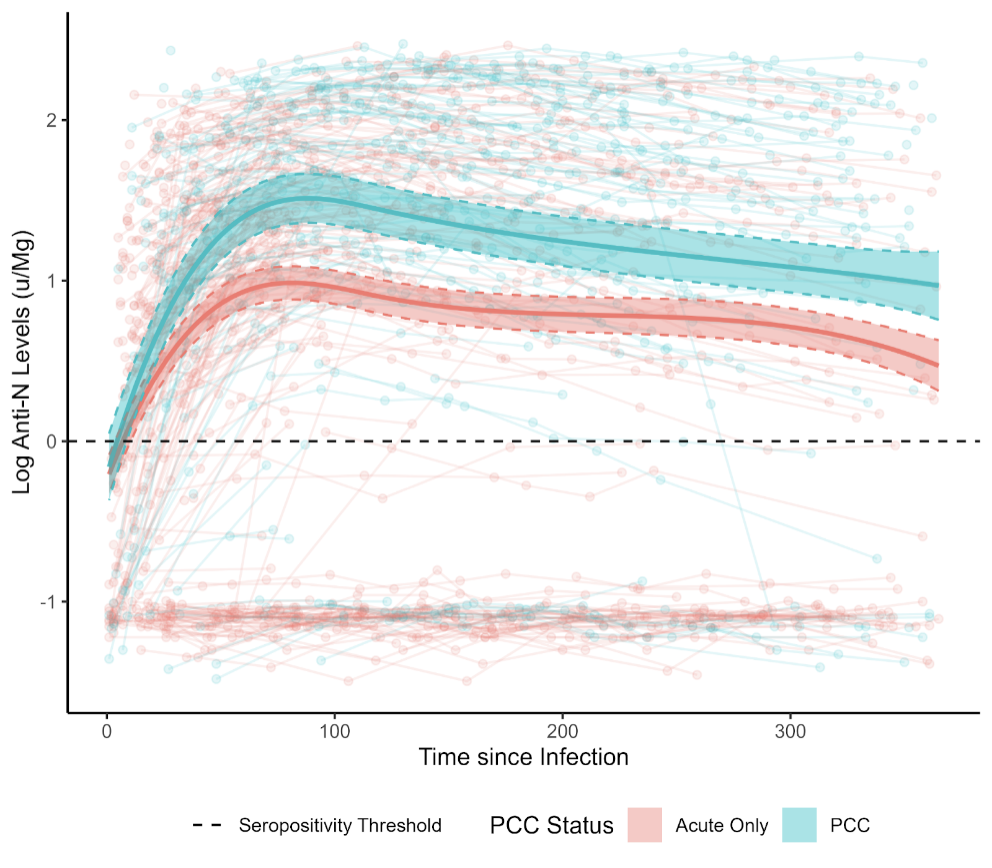
Note: People with Long Covid (Post-Covid Condition, PCC) are shown in blue and people without Long Covid are in red. The dots are individuals’ responses and the thick lines are the overall findings.
