Virus Watch preliminary findings on 22nd November 2020
Virus Watch is a research study run by University College London and the NHS. Virus Watch aims to identify how SARS-CoV-2 spreads, and how to stop it. The findings from the Virus Watch study presented on this page are early, preliminary results and should be interpreted with caution. We are presenting these early findings for participants, the general public and policy makers. No antibody or antigen swab testing results from Virus Watch are included as these parts of the study are not yet fully operational and we are still actively recruiting participants. These early data represent an example of how we will use the results of Virus Watch to identify how SARS-CoV-2 spreads, and how to stop it. A detailed description of the Virus Watch study and our detailed research questions can be found in our study protocol.
Table of contents
- Summary of findings so far
- Interpretation of findings
- Characteristics of people in Virus Watch
- Prevalence of symptoms
- Incidence of symptoms compared to 2018/19
- Activities in the week before a positive COVID test
- Number of contacts in people with a positive test
1. Summary of preliminary findings so far:
- Virus Watch began recruiting people in July 2020 and as of 22nd November, 20,920 households and 43,073 people across England and Wales have joined the study.
- The levels of people reporting cough, fever or loss or change to sense of smell and/or taste was highest in the week commencing 21st September 2020, with the highest level of symptoms reported in children and young adults aged 0 to 17 years.
- The levels of people reporting cough or fever in Virus Watch were lower for July, August, October and November 2020 compared to our prior studies on other infections conducted in 2018 and 2019.
- 242 people over the age of 16 in Virus Watch reported a positive COVID-19 test. Of these, 40% had close contact with other people outside the household in the 7 days prior to this test.
- In the period when they were likely to be contagious (two days before onset of symptoms until the illness survey date), 67% participants over the age of 16 with a positive COVID-19 test reported having no non-household contacts with whom they spent 15+ minutes within a 2 metre distance. 33% reported contact with other people.
- Of the 242 positive COVID-19 cases, 17% occurred in a one-person household and 83% in multi-person households. Of the 149 multi-person households where at least one case was reported, 70% reported a single case, while 30% reported multiple cases.
2. Interpretation of findings
Findings so far from Virus Watch are taken from over 43,000 people across England and Wales. People taking part are slightly older than the average age found in England and Wales, but the study contains over 6,000 children and young people under the age of 18. Our results indicate that the number of people with symptoms of cough, fever and loss or change to sense of smell and/or taste peaked in the week commencing 21st September 2020. We believe this peak was due to Rhinovirus as the timing and peak of symptoms in the 0-17 age group coincides with high levels of people testing positive for Rhinovirus in the Public Health England surveillance data.
We compared Virus Watch results on the number of people with cough or fever to data we collected in 2018/19 and found that levels of these symptoms in Virus Watch were lower for July, August, October and November across all age groups. Levels of cough or fever vary each year, but these lower levels compared to 2018/19 may be a result of physical distancing and hygiene measures that people in England and Wales are undertaking compared to previous years. This indicates that physical distancing and hygiene measures introduced in response to COVID-19 may have had an impact on the transmission of other respiratory infections.
We are providing summaries of our preliminary findings to inform public health action by working through our partnerships with Public Health England, NHS and to Government Scientific Advisory panels.
3. Characteristics of households and individuals in Virus Watch
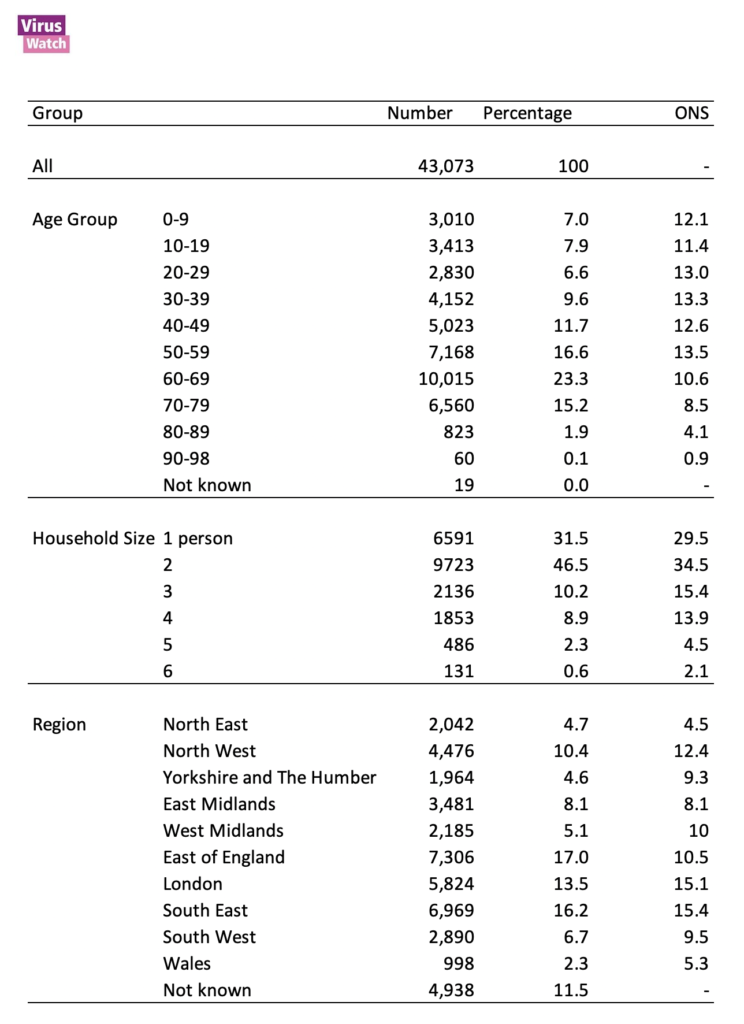
Virus Watch began recruiting people in July 2020 and on 22nd November there were 20,920 households and 43,073 people taking part in the Virus Watch across England and Wales (Table 1) with a median age of 54. Participants were recruited using a range of methods including a probability postal sample, social media, and SMS messages from General Practices.
Comparison with Office for National Statistics (ONS) data for the age distribution of the population in England and Wales in mid-2019 found that Virus Watch had relatively lower proportions of people aged 0-49, and higher proportions of people aged 50+ (Table 1). A total of 4,447 people from minority ethnic backgrounds are currently taking part in Virus Watch, and we are actively recruiting additional participants as part of the Virus Watch health equity study. There were people taking part in Virus Watch across 336 Local Authorities in England and Wales (Figure 1). Compared to ONS estimates for the population of England and Wales, a higher proportion of Virus Watch participants live in the East and South East of England and a lower proportion in the North West, Yorkshire, West Midlands, London, the South West, and Wales, with similar proportions to national figures for the North East and East Midlands (Table 1).
The majority of households in Virus Watch comprise one person (31.5%) or two people (46.5%); these proportions are similar to UK 2019 national estimates for one person households and higher for two person households. Compared to national estimates for the UK in 2019, Virus Watch comprises lower proportions of households with three or more members (Table 1).
Table 1: Participants in Virus Watch, 22nd November 2020
Notes:
- ONS = Office for National Statistics. ONS data for age and region drawn from Mid-2019 Estimates of the Population for the UK, England, and Wales, Scotland and Northern Ireland (figures for England and Wales only).
- ONS data for household size drawn from Families and Households in the UK 2019 (only UK wide estimates available).
Figure 1: Participants in Virus Watch by local authority district
4. Prevalence of cough, fever and loss or change to sense of smell and/or taste by week
The prevalence of symptoms of cough, fever and loss or change to sense of smell and/or taste across all age groups was highest in the week commencing 21st September 2020 at 3,795 per 100,000 (95% confidence intervals: 3,500 – 4,114) and has remained lower up to and including week commencing 9th November (Figure 2). The peak in this week commencing 21st September 2020 was mainly as a result of a large increase in symptoms in the 0-17 age group, with smaller peaks in 18-39 and 40-64 age groups (Figure 3). The peak seen in the week commencing 21st September 2020 coincides with a large number people testing positive for Rhinovirus in the Public Health England data mart surveillance results (see Figure 13 in this Public Health England report), suggesting this peak in symptoms of cough, fever and loss or change to sense of smell was likely driven by Rhinovirus and not SARS-CoV-2 (the virus responsible for COVID-19).
Figure 2. Weekly prevalence of cough, fever and loss or change to sense of smell and/or taste per 100,000 people with 95% confidence intervals.
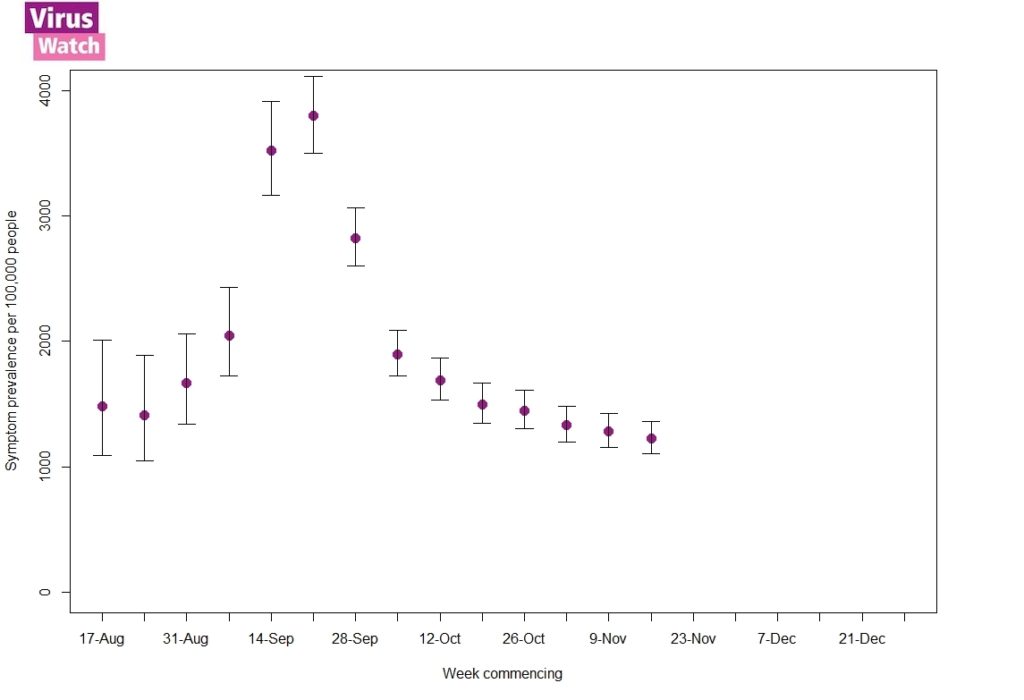
Figure 3. Weekly prevalence of cough, fever and loss or change to sense of smell and/or taste per 100,000 people by age group with 95% confidence intervals.
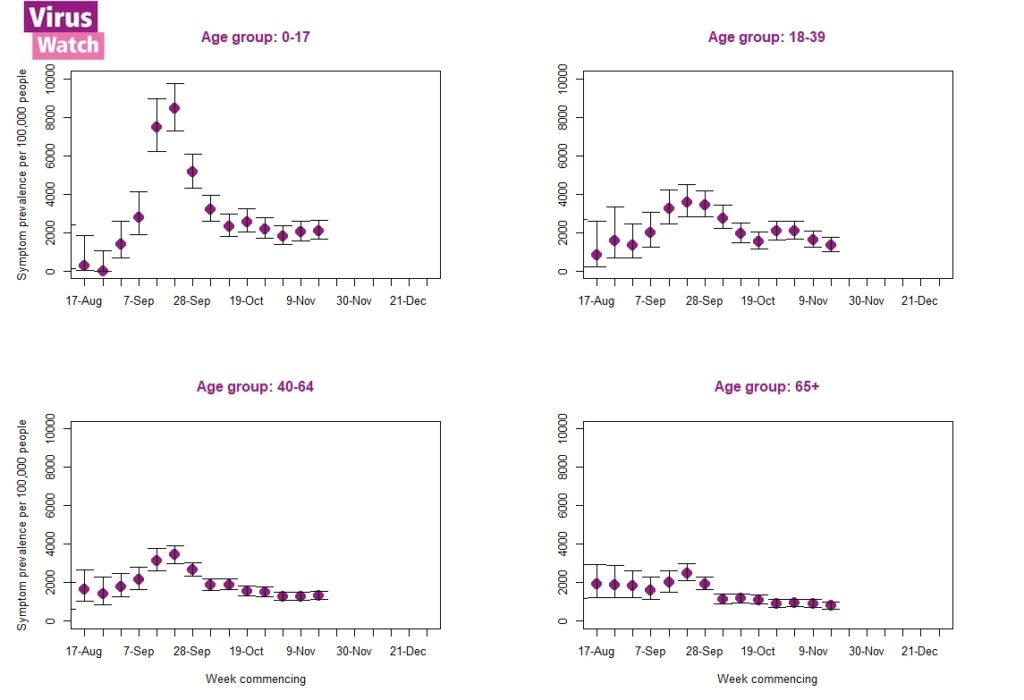
Notes:
- All results are provisional and subject to revision.
- These statistics refer to symptoms reported by Virus Watch participants in the community, by which we mean private households.
- Weekly prevalence rates used in these figures were calculated using the total number of people reporting to Virus Watch each week as the denominator, and the number of people reporting symptoms of cough fever and loss of smell or taste as the numerator.
- We excluded data from the first week of reporting for all participants.
5. Monthly incidence of cough and fever, weighted by region and sex in 2020 compared to 2018-2019 in England.
The Virus Watch study builds upon our previous research on investigating respiratory infections in the community. We have been able to estimate current levels of cough (dry cough or coughing up phlegm) and fever in Virus Watch participants and compare these with our results from the Bug Watch study that collected similar data in 2018-2019. Our estimates in Figure 4 have been adjusted by age, sex and geographical region of people in both studies. Our results show that compared to 2018-2019, there have been lower levels of cough and fever in July, August, October and November 2020. Symptom levels for July, August, October and November were lower for all age groups in 2020 compared to 2018-2019 as shown in Figure 5.
Figure 4. Monthly adjusted incidence rates of cough or fever per 100,000-person-week in England with 95% confidence intervals.
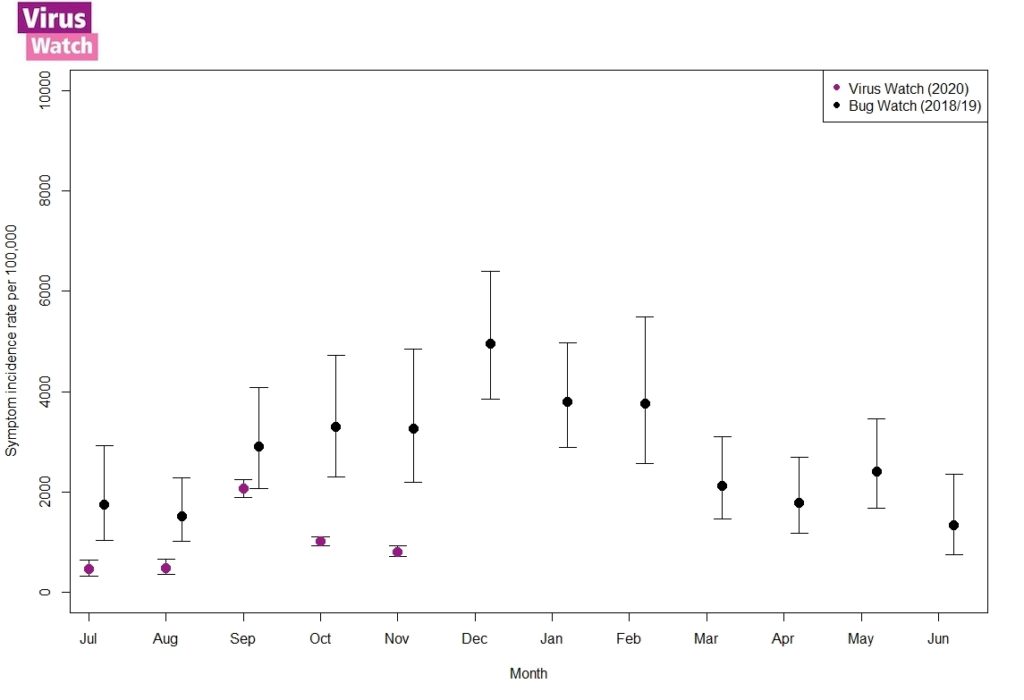
Notes:
- Adjusted by age, sex, and geographical region.
- All results are provisional and subject to revision.
- Weekly incidence rates used in these figures were calculated using the same methodology and statistical code that is available and reported here.
Figure 5. Age-stratified monthly adjusted incidence rates of cough or fever per 100,000-person-week in England with 95% confidence intervals.
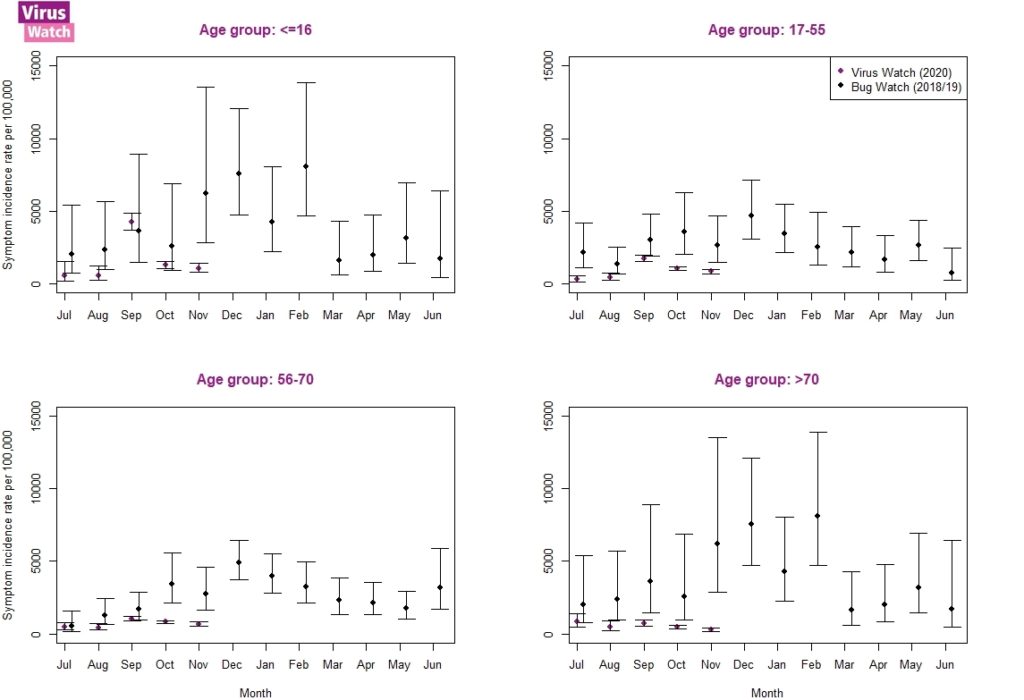
Notes:
- Adjusted by sex, and geographical region.
- All results are provisional and subject to revision.
- Weekly incidence rates used in these figures were calculated using the same methodology and statistical code that is available and reported here.
6. Activities in the week prior to testing positive
On 22nd November there were 242 incident cases of COVID-19 tested and reported by people aged 16 years or older taking part in Virus Watch. Tests reported by people in Virus Watch would mainly have been conducted in the NHS Test and Trace (Pillar 2 system) with some from the Public Health England (Pillar 1) systems. We asked people with a positive COVID-19 test about activities and events that they did in the seven days before anyone in the house became ill. A majority left home, with just over half having direct contact with another person outside the household and 40% having close contact. 70% of people wore a facemask or covering whilst out of the house. Caution is required when interpreting the results of Virus Watch activity data as they do not imply where or how people in Virus Watch were infected as this requires further more detailed analysis which is underway.
Figure 6. Activities reported in the 7 days prior to a positive COVID test for August to November in participants aged 16 and older with 95% confidence intervals.
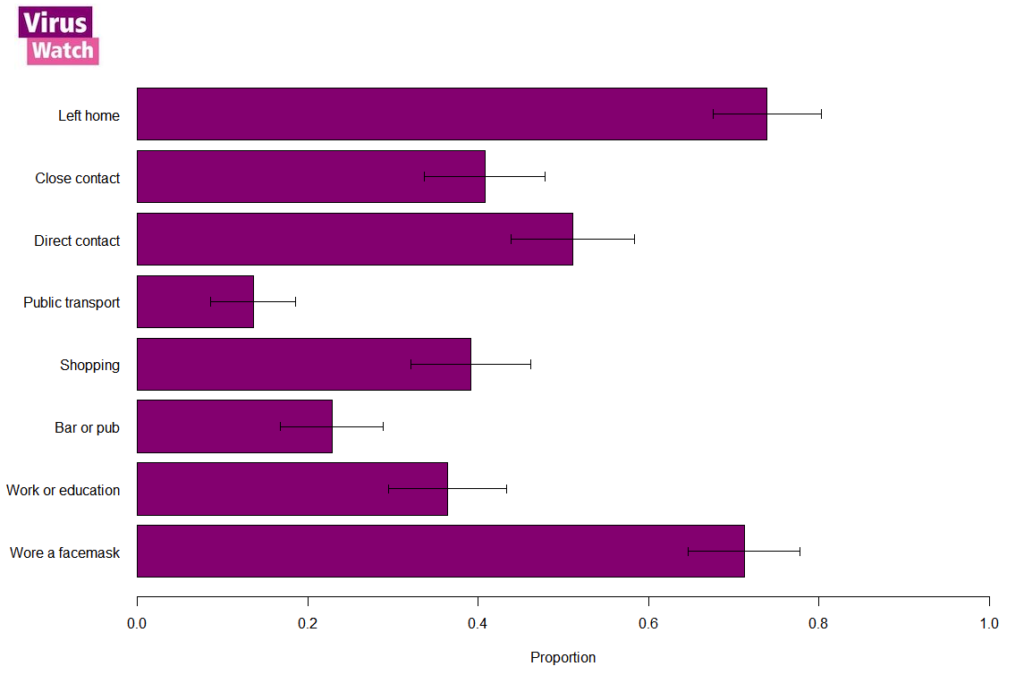
Terms used in figure:
- Left home – Leaving the house or flat for more than one hour
- Close contact – Having close contact with someone other than a household member – Close contacts are people who were within two metres of you for 15 minutes or more but who you did not talk to or touch
- Direct contact – Having direct contact with someone other than a household member. Direct contacts are people who you had physical contact with or talked to, within a 2 metre distance
- Public transport – Using any form of public transport
- Shopping – Spending more than half an hour on any day out shopping
- Bar or pub – Meeting others at a bar, pub, restaurant or party
- Work or education – Going to work or education outside the household
- Place of worship – Going to a place of worship
- Wore a facemask – Wearing a mask or face covering outside of the house
7. Number of contacts per person reporting a positive COVID test and household clustering.
We asked adults over the age 16 with a positive COVID-19 test about their number of contacts from the two days before their symptoms started to the time of their illness survey, excluding contact with other household members. People with COVID-19 are most likely to be contagious during this period. Of participants over the age of 16 with a positive COVID-19 test, 67% reported having no non-household contacts with whom they spent 15+ minutes within a 2 metre distance, while 33% reported contact with other people.
Of the 242 COVID-19 positive cases, 17% occurred in a one-person household and 83% in multi-person households. Of the 149 multi-person households where at least one case was reported, 70% reported a single case, while 30% reported multiple cases within a two week period of one another. Please note that because we are still actively recruiting for Virus Watch, we do not have complete two week follow up for all households and consequently this may be an under-estimate of how many households experience multiple cases. We will be able to provide complete follow-up and more detail about household clustering in future when results from Virus Watch swab tests become available.